The estimated cost of delayed discharges in the United Kingdom alone exceeds £900 million per year. In Australia, exit block costs reach upwards of $2 billion just for patients needing appropriate aged care and disability support.
Patient flow is defined as the movement of patients through various stages of healthcare delivery, from the initial point of contact with the healthcare system to the discharge or transfer. Slow patient flow creates a ripple effect of consequences throughout the care journey, including overcrowding, inefficient use of resources, increased risk of medical errors, patient dissatisfaction, and high costs.
As the demand for healthcare increases, capacity is struggling to keep pace, making it more difficult for healthcare systems to manage this balancing act. Targeting patient flow has been proven to decrease patients’ length of stay (LoS) and increase the speed with which patients are processed toward discharge. However, as a process that differs by organisation and by patient, the solution can often remain elusive. In this article, we discuss the challenges of addressing patient flow and present our philosophy of flow, which has three key principles:
1. Look backwards along the patient flow journey;
2. Provide tools to create transparency of demand;
3. Focus on digitising clinical workflows and sharing real-time updates.
‘Ramps’ to address in order to improve patient flow
Ambulance ramping – or queuing – has become a key issue for healthcare services, compromising patient safety, exhausting care teams, not to mention causing a media and political frenzy. In the past year alone, there have been dozens of news articles highlighting the issues with ramping.
In Australia, the AMA recently published their 2023 Ambulance Ramping Report Card showing every state and territory falling short of their ambulance ramping performance targets. The report highlights that 1 in 4 patients arrive at the ED by ambulance, and that every state has deteriorating performance against a backdrop of consistent annual increases in the number of incidents requiring ambulances.
A similar scenario is present in the UK, with a reported 237,000 ambulance handover delays exceeding 15 minutes in October 2023, resulting in 149,000 hours lost. Even more troubling, an estimated 37,000 patients experienced potential harm as a result of hour-plus handover delays that month.
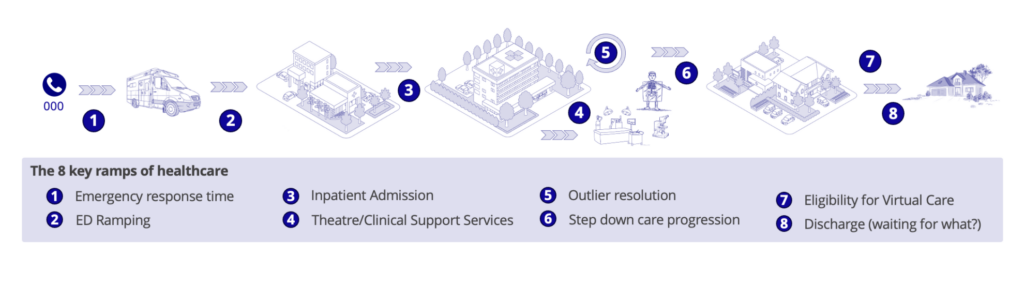
The natural reaction to these challenges is to focus on the healthcare system’s ‘front door’ where ambulances ramp as they arrive to transfer patient care to the emergency department. However, we can’t simply throw more volume at the front door and expect the system to absorb it, especially if that system lacks the tools to understand demand and has fixed constraints that impede flexibility to increase throughput. Whilst the challenge of bed capacity is most evident in the ED, it is also present along the whole healthcare value chain. The diagram below highlights 8 of the core ‘ramps’ or pinch points which need to be addressed to optimise patient flow.
Lessons from Lean manufacturing
Resolving ‘flow’ challenges has long been the focus in manufacturing and supply chain management, and there is an opportunity to take learnings from these industries and apply them to healthcare. The concept of ‘flow’ is central to Lean thinking, in that overproduction at any part of a production line drives inefficiency. In Lean manufacturing, the goal is to have each part of the production line operating in concert, and to scale activities up or down in order to optimise ‘flow’.
Whilst it may seem questionable to some to compare a healthcare system to a manufacturing line, the principle of ‘flow’ is consistent across both industries. Evidence supports that Lean techniques and tools are increasingly being applied in healthcare organisations for improving safety, efficiency, and quality, optimising the workflow in healthcare services and improving ED operations. Those organisations that have adapted the teachings from Lean manufacturing to their systems and processes report reduced waiting and reduced LoS, better utilisation of resources, and timely release of capacity for next use.
So, how can we address the challenges in our emergency departments in the context of increasing volumes, constrained capacity and funding, and exhausted care workers? This brings us to our philosophy of flow.
Look backwards along the patient flow journey
Looking backwards along the patient flow journey may seem counterintuitive at first. The noise is in the ED and on the ramp – this is where the media and the politicians are looking, and it is easy to follow the noise. However, this is not where the heart of the problem lies.
As we look downstream, we see issues with getting patients out of ED and into an inpatient bed. Further along is the issue with completing transfers and resolving outliers. And further still we run into challenges with addressing moves to sub-acute or step-down care. Equally we have challenges with transitioning patients to virtual care services, and for certain cohorts with discharge.
As we study each of these issues in more detail it becomes clear that solving problems with ED by adding capacity or staff will provide short term relief and meet the immediate needs of patients; however, within a short time the ‘flow’ challenge will move along to the next bottleneck – admitting patients into the hospital. This problem repeats, moving the flow blockage to the next problem downstream.
Solving any one of these challenges simply moves the problem downstream, without releasing capacity in the system. For anyone who understands baseball, the comparison can be made to moving between the bases. A score is only recorded when you get around the diamond, you don’t get anything for moving from base to base other than a loaded field.
However, if you work backwards along the patient flow journey, and resolve the ‘stranded patient issue’, and the numerous ‘waiting for what’ and ‘discharge barriers’, the ripple effect creates capacity in the system. This allows the resolution of outliers and awaiting patient transfers, which in turn releases capacity to take in patients from ED who are waiting for a bed.
Provide tools to create transparency of demand
Being able to ‘see’ demand across the eight ramps previously mentioned is essential for addressing operational challenges like understaffing and resource allocation. Dependency on paper tools and excel files severely limits a ‘whole of organisation’ approach to managing patient flow and increases the risk of inefficient bed allocation, delays to transfers and ward discharges and delays to overall bed access for elective, planned and urgent admissions.
Electronic patient journey boards offer real-time visibility into patient status, treatment progress, and bed availability, allowing healthcare teams to anticipate and address patient needs more effectively.
A recent study conducted by Monash University explored the effectiveness of electronic patient journey boards for improving patient flow at Alfred Health. The study found that staff felt visibility of information had increased. In addition, the study found the alignment of patient flow management strategies transitioned from 30 disparate approaches to just 9 variations closely mapped to clinical workflows. This not only enhanced the availability and consistency of patient information throughout the service but also streamlined operational efficiency.
At an enterprise-level, operational command centres focus on releasing capacity and the identification of potentially vulnerable patients to help organisations optimise resource management within individual facilities or across the integrated care system. One study of a centralised coordination hub used to manage patient flow across acute tertiary care concluded, “Visibility of the comprehensive end-to-end data allows everyone to have a common understanding of the pressure points and opportunities to ease flow or create capacity and supports the staff to be accountable for the decisions they make.
Advancements in artificial intelligence are introducing tools like predictive analytics that allow healthcare organisations to look at expected presentations and subsequent inpatient admissions to proactively manage flow.
Focus on digitising clinical workflows and sharing real-time updates
Returning to the teachings from Lean manufacturing, real-time data is crucial for predictive insights and operational agility. It allows healthcare organisations to anticipate and address bottlenecks in patient flow by adapting their resources and workflows to meet both current and future demands. Additionally, research suggests a mutually beneficial relationship between Lean principles and technological advancements, where Lean methodologies facilitate more seamless adoption of new technologies, which in turn, enhance the effectiveness of Lean practices.
The digitisation of clinical workflows involves implementing technology-driven solutions like electronic patient records (EPRs), clinical noting tools, and inventory management systems to reduce manual errors, eliminate paper-based inefficiencies, and boost staff productivity. Streamlining these workflows aligns with Lean manufacturing’s lessons about waste.
Real-time data analytics complement workflow automation by providing timely insights into key performance metrics such as patient volumes, wait times, bed availability, and staff allocation. Access to this data empowers healthcare providers to make informed decisions as patient care unfolds.
Philosophy into practice
Alcidion offers a modular approach to address patient flow challenges, which enables organisations to discretely target the identified eight ramps by using strategies and lessons from Lean manufacturing. By using innovative solutions such as electronic patient journey boards and predictive dashboards, Alcidion enables healthcare providers to optimise efficiency and increase patient throughput. Embracing this philosophy not only streamlines workflows but also fosters a more responsive and patient-centred healthcare system, ensuring sustainable success in a strained environment.
Explore how organisations across Australia, New Zealand, and the UK have successfully tackled patient flow challenges using our philosophy of flow.