Scotland’s cancer waiting times
You’ve been referred to the urgent suspicion of cancer (USC) pathway by your GP because they suspect your mole might be skin cancer. While it’s worrying, you can take some comfort in knowing you’ll be treated within 2 months as per the 62-day standard… or so you think.
The latest Public Health Scotland cancer waiting time figures paint a different picture. It’s a bleak reality; for the past year, all NHS boards have repeatedly missed the 62-day standard except for 1 Health Board that met the key target between January 1st and June 30th, 2022.
A patient’s nightmare experience
Imagine the stress of worrying about skin cancer and not being able to receive treatment in time. It’s frustrating enough waiting for an appointment, but it’s even worse when the hospital fails to coordinate your care properly.
After receiving a text with your appointment date, you’re relieved, but a day before your appointment, you receive another text saying it’s cancelled. You follow up and find out it was a “glitch in the system” and your appointment hasn’t been cancelled. What if you hadn’t followed up?
You go to your appointment, but their system glitches again and they lose your dermoscopic image. The dermatologist doesn’t have access to your high-resolution lesion images, so what does he do? He takes a picture with his phone. It’s definitely not high-resolution, and as the saying goes, “when in doubt, cut it out”, and they were certainly in doubt, so they removed the lesion only to later discover it was completely harmless.
Regrettably, some patients don’t need to imagine this as they have lived it.* With the escalating cases of skin cancer in Scotland, this unfortunate reality is set to become increasingly prevalent.
Are dermatologists equipped to handle the soaring cases?
Skin cancer is one of the most common types of cancer. Every year, around 12,000 people in Scotland are diagnosed with non-melanoma skin cancer, and around 1,200 malignant melanoma cases are reported annually. And over the past decade, cases for skin cancer have increased by 37%.
On top of the impact on patients, the diagnosis and management of suspected skin cancer takes over 50% of a specialist dermatology service workload. How are the 876 dermatologists working in the UK supposed to manage those numbers?
Consultant dermatologists believe teledermatology is one of the most effective solutions available. It can improve patients’ access to care with the ability to increase the capacity of the workforce by enabling digital triaging, diagnosis, monitoring, or assessment of skin conditions remotely. A robust digital solution for dermatology coordination is urgently needed to truly enhance patient care.
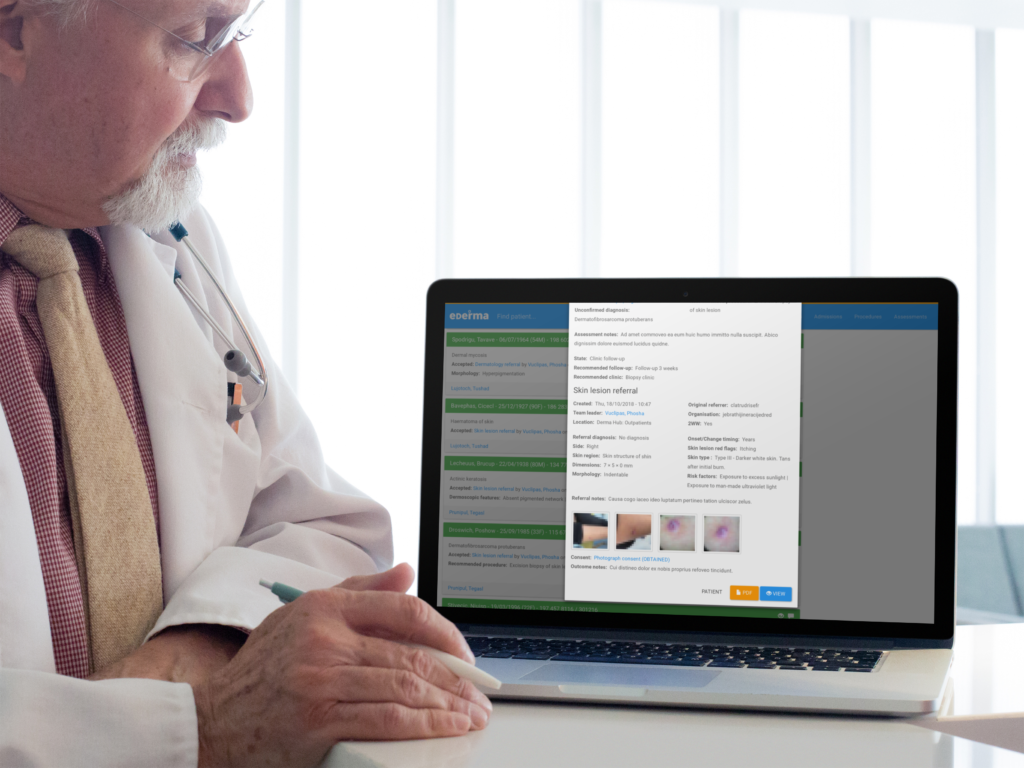
Open Medical’s digital solution, PathpointⓇ eDerma, has gone above and beyond teledermatology, and already enabled healthcare organisations to achieve remarkable outcomes.
More than teledermatology
Open Medical’s Director of Innovation, Piyush Mahapatra, shared some incredible results achieved by a hospital using eDerma within just 2 months. Prior to eDerma, less than 1% of their patients were assessed within 2 weeks of a potential skin cancer referral. Now, 99% of patients were assessed by a consultant dermatologist within 2 weeks, and over half received a diagnosis or treatment decision in just 14 days, as per diagnostic standards.
eDerma’s success in helping to decrease skin cancer waiting times is remarkable and showcases the enormous potential for digital solutions to revolutionise skin cancer pathways. The platform has transformed dermatology workflows by providing a clinician-centred service that addresses every need throughout the entire patient journey. eDerma’s cloud-based, clinically coded, and customisable digital platform creates efficiency, saves staff time, provides patients with prompt specialist care, increases the capacity for physical consultations for those who desperately need it, but what really sets eDerma apart is its ability to be configured to fit any clinical workflow.
eDerma has been implemented throughout various healthcare organisations, and each eDerma model is unique. A “one-size-fits-all” approach simply won’t work; the key is to listen to the end-users and understand the challenges at the grass-root level. With eDerma, healthcare professionals can collaborate seamlessly, providing the highest level of care to their patients and ultimately, saving lives by offering early diagnosis and treatment.
*Disclaimer: the patient’s experience is based on a real story.
Open Medical will be exhibiting at the FutureScot Health and Care Transformation Conference stand 5 on March 30th. We would be delighted to hear your thoughts on digital transformation solutions, from enhancing dermatology workflows to transforming any aspect within the clinical setting.